Article
Proposed rule: Look for changes to MIPS, supervision of APPs
Author(s):
"The much-anticipated proposed rule for the Medicare physician fee schedule was finally released on July 29, 2019. The bottom-line impact to urology for 2020-based changes to relative value units is a projected +1% additionally," write the Painters.
thicha - stock.adobe.com


Ray Painter, MD

Mark Painter
The much-anticipated proposed rule for the Medicare physician fee schedule was finally released on July 29, 2019. The bottom-line impact to urology for 2020-based changes to relative value units (RVUs) is a projected +1% additionally. The Centers for Medicare & Medicaid Services is projecting a minor 0.14% increase in the conversion factor from $36.04 to $36.09.
While the overall impact on the specialty for 2020 is minor, there are a few changes of note that we will address in this article. The more newsworthy information in the proposed rule surrounds changes to evaluation and management (E/M) coding effective Jan. 1, 2021.
More from the Painters - Chart reviews: Make these changes to prevent payer mistakes
First, we will address the changes for 2020.
MIPS changes. In the area of the Quality Payment Program (QPP), Medicare is proposing to increase the requirements for the Merit-based Incentive Payment System (MIPS) program. The threshold for physicians to avoid penalties for payments in 2022 will require a minimum score of 45 for performance in 2020, up from 30 in 2019. The percentage assigned to the Quality and Cost categories will be adjusted to 40% and 20%, respectively. The minimum score for exceptional performers will be raised to 80 points.
CMS did not change the eligibility requirements for reporting year 2020. The maximum penalty for those failing to meet MIPS requirements has been increased to –9%, up from –7%. Penalties and bonuses will be applied to payments in 2022 based on 2020 reporting. We encourage you to further review the proposed changes for the QPP program as CMS continues to change this program to increase the incentives to participate.
Supervision of advanced practice providers. CMS is proposing to modify regulation of physician supervision of physician assistants (PAs) to give PAs greater flexibility to practice more broadly in the current health care system in accordance with state law and state scope of practice. The proposal includes a provision that, in the absence of state law governing physician supervision of PA services, the physician supervision required by Medicare for PA services would be evidenced by documentation in the medical record of the PA’s approach to working with physicians in furnishing their services.
Physical therapy/occupational therapy benefits. CMS is proposing a change in per-beneficiary incurred expenses under physical therapy definitions. These benefit caps are no longer applied as limitations but as threshold amounts above which services require, as a condition of payment, inclusion of modifier –KX, and that use of modifier –KX confirms that the services are medically necessary as justified by appropriate documentation in the patient’s medical record. The definitional change should assist in providing services to patients receiving benefit from ongoing physical therapy-type services for pelvic floor rehabilitation. Functionally, you will need to continue to document medical necessity and improvement and use modifier –KX to indicate the services provided are medically necessary.
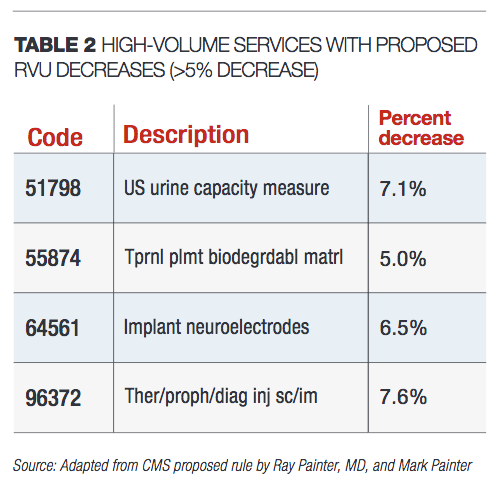
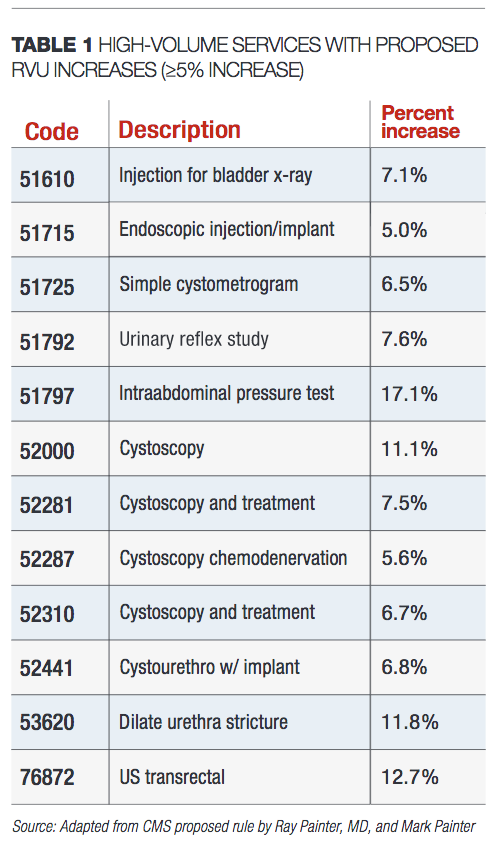
RVU changes. Table 1 includes a few higher volume services for which the proposed RVU changes will result in increases of greater than or equal to 5% in the office setting beginning Jan. 1, 2020 if adopted. Table 2 includes a few higher volume services for which the proposed RVU changes will result in decreases of greater than 5% beginning Jan. 1, 2020 if adopted.
The majority of the changes reflect changes to the practice expense values based on adjustments to equipment valuation and/or disposables related to the procedure.
Changes to some specific high-volume codes are noteworthy. The work values for the UroLift system codes 52441 (initial implant) and 52442 were reduced from 4.5 to 4 and 1.2 to 1.01, respectively. However, the non-facility value for each code was increased, resulting in an overall increase when the service is performed in the office. For 52441, the increase in the office-based payment as proposed is 6.8% as noted in Table 1, and the increase in office-based payment for 52442 as proposed is 4.6%.
In addition, code 54640 (Orchiopexy, inguinal approach, with or without hernia repair) is proposed to have a reduction of 9.7% in the facility setting, reflecting a code change eliminating the “with or without hernia repair” language.
Next: Looking ahead to 2021Looking ahead to 2021
E/M changes. The biggest news included in the proposed rule does not take effect on Jan. 1, 2020 but rather is scheduled to be effective Jan. 1, 2021. As noted in our August 2018 column (“Medicare proposed rule outlines significant changes,” page 26), CMS proposed a radical change to payment and documentation for E/M codes. In our December 2018 column (“Medicare final rule: How E/M changes help urologists,” page 31), we addressed the CMS finalized rule to change the payments and documentation requirements for E/M codes effective Jan. 1, 2021. The changes would have consolidated payments for new and established patient office visits to three levels for each category.
The news was met with a decidedly mixed reaction. In response to the proposed and final rule, the American Medical Association CPT Editorial Panel and Relative Value Update Committee convened work groups and expanded surveys to revise the structure of the E/M service codes. The results of these efforts were reported to CMS. In this proposed rule, CMS is proposing to accept the majority of the work done by the AMA.
Read -Working with a co-surgeon: How should procedures be billed?
Practices, EHRs, and other entities will now have a little over a year to adapt to the changes in office/outpatient E/M visits. We will spend more time addressing these changes over the next year but present a quick summary of the changes below. (Note that these changes will not affect coding, payment, or documentation requirements for 2020. For 2020, continue to follow rules adopted for 2019.)
• CPT code 99201 (Level 1 new patient office/outpatient E/M visit) is being eliminated.
• History and physical examination will no longer affect code selection but should be documented as appropriate. This change will likely require some changes to your EHR templates for both. Medicine reconciliation will still be required under MIPS, but review of systems and other portions relative to past medical, family, and social history can be changed to reflect more focused and relevant information with updates as needed for clinical reasons. For the physical examination, vitals will still be required for MIPS, but you will no longer need to include observations for eight systems or bullets as required by 1997 guidelines and instead can focus on documentation of only those issues relevant to patient care.
• Medical decision-making changes are subtle but will need to be addressed in how you think about the level of service you are charging. The AMA will eliminate some of the more ambiguous language from the table of risk. Data as noted in MDM will be revised to focus more on volume of relevant information and summation effort required and less on counting the amount of data reviewed.
• Time will be the other option for selection of service level. There are a number of changes surrounding time-based coding. Time will now be considered to be total time spent on that day, eliminating the face-to-face component with regard to time. In addition, the requirement for the visit to include 50% spent in counseling or coordination of care will be eliminated. Time can be used to document any visit if you document the time spent that day.
• CPT code definitions will include time ranges within the code definition, eliminating the ambiguity of the average visit time associated with current coding rules. The times for each code as noted in the rule are as follows: 99202 (15-29 minutes), 99203 (30-44 minutes), 99204 (49-59 minutes), 99205 (60-74 minutes), 99212 (10-19 minutes), 99213 (20-29 minutes), 99214 (30-39 minutes), and 99215 (40-54 minutes). A new code will be added to the CPT manual to report time for services that exceed level 5 services: 99XXX for each additional 15 minutes over 74 minutes for 99205 and 54 minutes for 99215.
• CPT codes 99358-9 (Prolonged E/M without Direct Patient Contact) would no longer be reportable in association or “conjunction” with office/outpatient E/M visits.
• A new add-on code will be added to CPT to address patients who have chronic issues addressed during a visit. The code can be used by any specialty.
• All codes will be revalued with slight increases. The overall impact to urology is projected as an increase of 8%.
Comments on the proposed rule are encouraged and must be submitted by Sept. 27, 2019. Comments may be submitted electronically (www.regulations.gov), by regular mail, or by express or overnight mail.
The information in this column is designed to be authoritative, and every effort has been made to ensure its accuracy at the time it was written. However, readers are encouraged to check with their individual carrier or private payers for updates and to confirm that this information conforms to their specific rules.

















