Defining PSA Nadir After Definitive Therapy in Prostate Cancer
Brian Helfand, MD, PhD, describes the ways in which the PSA nadir can be defined after definitive therapy and the implications of the definition used for patients with prostate cancer.
Episodes in this series
Raoul S. Concepcion, MD, FACS: Brian, how do you define PSA [prostate-specific antigen] nadirs, because I think this is an important point, in the surgical patient and in the radiotherapy patient?
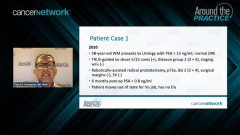
Brian Helfand, MD, PhD: Ultimately after surgery, when we take out the entire prostate, we’re really expecting that PSA to go to a value of undetectable, 0 [ng/mL]. There are certain definitions, because we use ultrasensitive assays, etc. For the most part, we want to see that at what an equivalent value is of 0 [ng/mL]. At our institution, that is less than 0.02, or less than 0.001 [ng/mL], which I have seen depending on the assay. If after surgery that level rises to a value of 0.2 [ng/mL], I think everyone would agree this is a common definition that would be considered a recurrence. There has been some evolution, especially for men with higher-risk disease, that if you’re using an ultrasensitive assay and you are seeing consecutive rises of that PSA before they’re actually getting to a value of 0.2 [ng/mL], most people would agree that that’s a recurrence as well. There is some devil in the details there, but certainly, I think if you’re going to walk away with this, the value of 0.2 [ng/mL] after a surgery would be considered a recurrence.
For radiation, it becomes a little trickier because we still have the prostate gland that’s in situ, and there is some benign tissue there, so there is for many patients, a level of PSA that exists. Your PSA will get down to some lowest value, or that nadir value. There have been various definitions that have been used throughout the years. I typically use what’s referred to as the Phoenix definition, which is a value of 2 ng/mL greater than their lowest value. Again, if you see consecutive rises at least a month apart, consistently rising more than would be expected, I also have some suspicion there that earlier intervention or recurrence may be warranted.
Raoul S. Concepcion, MD, FACS: Judd, we know that in the surgical patient, that nadir happens quickly, usually within 6 months, if it’s going to get to the level that Brian was discussing. What about with the radiation? When do you start to say, “OK, I’m at 6 months, I’m at 12 months, or I’m at 18 months?” When do you feel comfortable? I think as Brian pointed out, it’s not going to go to less than .001 or less than .02 [ng/mL]. What does that time frame look like in the radiation patient?
Judd W. Moul, MD: That’s a great question. In the classic teaching, in the era before androgen deprivation therapy [ADT] was used with radiation, the radiation therapy itself would sometimes take up to 18 months to clear the prostate cancer. Therefore, we’ve been always taught that you need to sometimes wait up to 18 months if it’s a patient who’s just receiving radiation, and you wouldn’t necessarily want to do a biopsy. You also have a PSA bounce phenomenon that sometimes can occur. Now, all the high-risk patients and many of the intermediate-risk patients are also receiving ADT with the radiotherapy. With the ADT, their PSA should go down generally more quickly, especially if you’re using an antagonist like Degarelix, or now the new oral option, relugolix. In general, the PSA typically nadirs, I see it nadir usually within 3 to 6 months in men who are getting hormone therapy with radiation.
The only additional point that I would make is that sometimes in guys who had low-risk or intermediate-risk disease and had a modern-era radical prostatectomy [RP] with aggressive nerve sparing, bladder neck sparing, and urethra sparing, we see low levels of PSA that are not cancer-related. Therefore, I agree with Brian that in the high-risk patients, you can jump on a PSA recurrence quickly, but I would caution the oncologists in our audience tonight that you must look at the RP pathology. Moreover, if it was not so bad pathology, and if the guy has a PSA of 0.13, or even 0.2 [ng/mL] a couple of years out, I tend to follow those patients because there is this phenomenon of benign glands at the margin. We know from the Mayo Clinic’s series and our work at Duke [Cancer Center], that honestly, sometimes up to 30% of patients can have this in long-term follow-up, a little bit of PSA in the system that’s not cancer-related.
Transcript edited for clarity.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.