Article
Radiation therapy for testis cancer increases secondary malignancy risk
Testicular cancer patients who are exposed to radiotherapy have a greater risk of being diagnosed with a subsequent non-testicular cancer, including bladder cancer.
Key Points
Chicago-Testicular cancer patients who are exposed to radiotherapy have a greater risk of being diagnosed with a subsequent non-testicular cancer, including bladder cancer, two groups of researchers reported at the American Society of Clinical Oncology annual meeting.
In one study, researchers from Virginia Mason Medical Center, Seattle found an increased risk of solid or blood-based tumors in testicular cancer patients receiving radiotherapy compared to those not exposed to radiotherapy. A European group reported similar findings, but noted that the increased risk of secondary malignancies does not translate into an increased risk of death.
"We specifically saw increases in thyroid, pancreas, upper-tract urothelial cancers, bladder cancer, and all hematologic malignancies-specifically, non-Hodgkin's lymphoma-and these risks were increased as time went on," said Daniel Lewinshtein, MD, a Society of Urologic Oncology fellow at Virginia Mason working with Christopher Porter, MD.

The age-adjusted and decade-adjusted overall rates of secondary malignancies were calculated, specifically in those patients who received radiotherapy. The same analysis was performed in a group of patients with stage I seminoma. The incidence rates of various malignancies, adjusting for latency time after testicular cancer diagnosis, were calculated and compared to rates published by SEER for the general population.
There were 15,362 patients diagnosed with testicular cancer who were followed for a total of 128,126 person-years; median follow up was 13.0 years.
Higher rates of non-Hodgkin's lymphoma
The calculated rate of non-Hodgkin's lymphoma was 40.2 cases per 100,000 persons per year for all testicular cancer patients who received radiotherapy, which was 53% higher than the national average. Patients not exposed to radiation did not have significantly increased rates of non-Hodgkin's lymphoma.
"Initially, there was increased risk for both patients who did and didn't have radiation compared to the general population, but as time went on, the risk of having a secondary malignancy in patients exposed to radiation treatment increased significantly compared to the general population," Dr. Lewinshtein said.
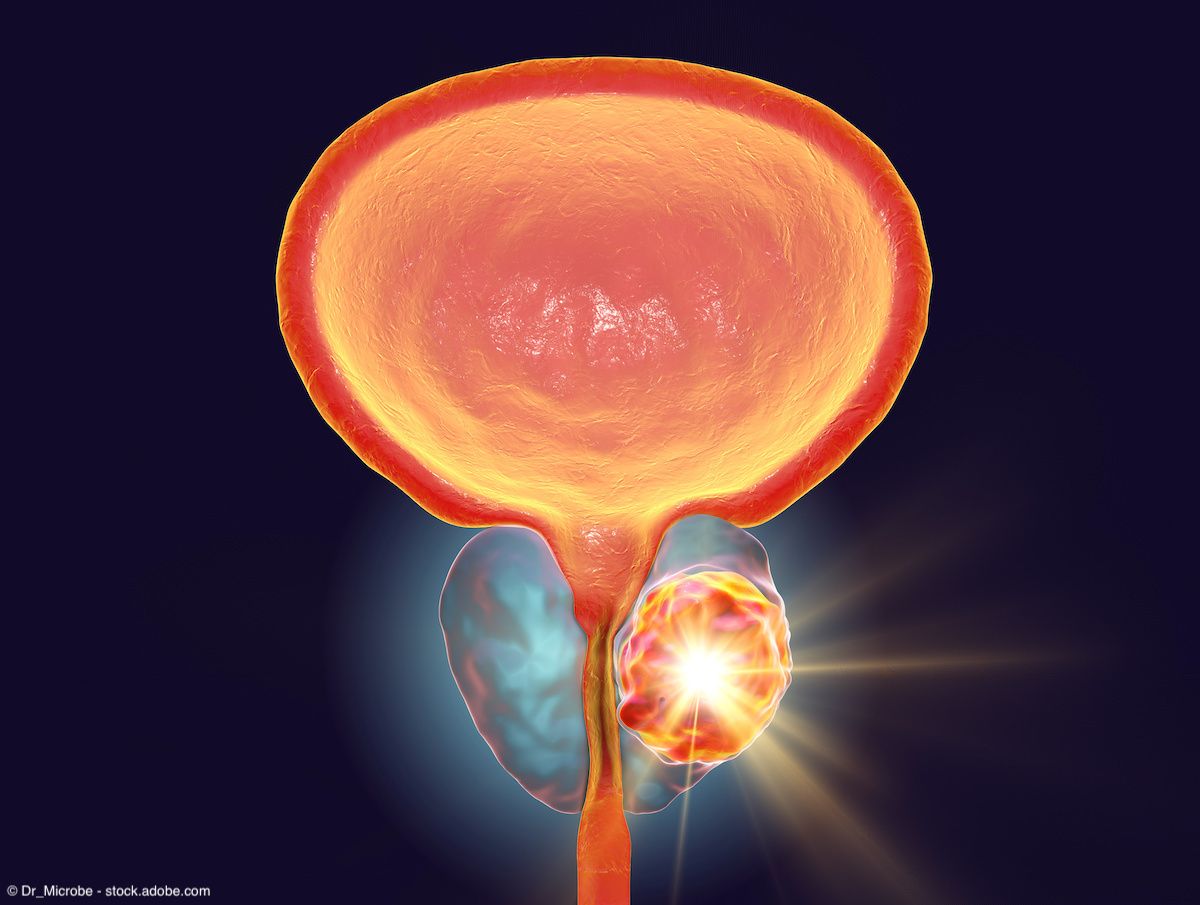
The calculated rate of bladder cancer was 52.6 cases per 100,000 persons per year for testicular cancer patients who received radiotherapy, which was 71% higher than the national average. Patients not exposed to radiation did not have significantly increased rates of bladder cancer.

"Essentially, there seems to be a real risk of secondary cancers in testicular cancer patients exposed to radiation, and patients should be counseled about these long-term risks," Dr. Lewinshtein said.
In the second study, researchers evaluating men from the United Kingdom and Norway found a similar increased risk of secondary malignancies in radiotherapy-treated men, although it does not affect mortality risk of death, first author Alan Horwich, MD, reported.
Dr. Horwich and colleagues identified 2,683 survivors (mean age of 39 years at diagnosis) of stage I seminoma from the UK and Norway who were treated with infradiaphragmatic radiotherapy. They were followed for a median of 17.7 years for secondary cancers and survival. The expected number of cancers was calculated using population rates of cancer incidence in Norway, England, and Wales.
"A young adult population and a highly curable illness means that we have a large number of men with long follow-up in whom to assess the risks of treatment," said Dr. Horwich, professor of radiotherapy at the Institute of Cancer Research, Royal Marsden Hospital, London and Surrey, UK.
Total person-years at risk were 52,000, during which there were 404 second cancers reported in 367 men and 698 deaths.
Radiotherapy was associated with an increased risk of other cancers, especially those in the abdomen.
"There was about 1.3 times the expected rate of developing other cancers. Slightly surprisingly, when we looked at the overall survival of the patients, their survival was not compromised, so that people cured of seminoma in this way lived just as long as people who never had testicular cancer, despite this increased risk of second cancers," Dr. Horwich said.
Sites with statistically significant excess risk were the bladder (42 observed, 19.5 expected; p<.0001), pancreas (20 observed, 8.3 expected; p<.001), stomach (23 observed, 13.7 expected; p<.03), and all abdomen-pelvic cancers (212 observed; 151.2 expected; p<.0001).
No relationship between risk of second cancers and radiotherapy dose was observed.
The patients are continuing to be followed.
"Some radiation-induced cancer problems can be very delayed," Dr. Horwich said. "If we look at the risk of developing a second cancer with time after treatment, we see that it's a rising risk. So we don't feel that this is the final analysis of this cohort.
"The trend in this illness now is to avoid radiation. We have good alternatives for managing patients with stage I seminoma. We can either manage them by observation alone, and only treat those who recur; that seems very safe. The alternative, instead of radiation to reduce the risk of recurrence, is the use of carboplatin, where just a single cycle of a relatively nontoxic anticancer drug seems to reduce cancer risk at least as effectively as does radiotherapy. Now, in the UK, radiotherapy is hardly used in these patients because of the second cancer incidence."