Treating Oligometastatic Prostate Cancer
Episodes in this series

[Transcript]
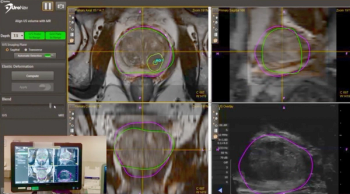
Jahan Aghalar, MD: The other role where sometimes a novel tracer may or may not impact outcomes is the treatment of oligometastatic disease. What do you do with a patient who has a slowly rising PSA [prostate-specific antigen]? You get the PET [positron emission tomography] Axumin scan, and you see 1 side of disease on PET L4. Do you go after it? Do you ablate it with radiation? Are we going to impact the trajectory of the disease? In those settings it brings up some interesting questions that will be brought up within the examination room and also hopefully within the realm of research.
Raoul Concepcion, MD, FACS: So Paul, Jahan brings up an interesting point. This concept-and I think this is going to become a bigger dilemma, especially for the busy clinical urologist-of oligometastatic disease at diagnosis. What do you do with the primary? The current definition by most people, although it’s not standardized, is less than 5 METs. Now we have the primary to deal with, we have mechanistically some different agents, and we have radiation. How do you see that playing out, basically with oligometastatic disease? Because we’ve talked about the deleterious effects of ADT [androgen deprivation therapy]. People necessarily don’t want to stay on long-term ADT, so for these patients, have you been using some of this next-generation imaging? How have you chosen? If you find somebody with a biochemical recurrence who, as Jahan said, maybe has an isolated lymph node that maybe you can go after. Are you going after them surgically and [spare] the patient ADT?
Paul Sieber, MD: Yes and no. If I have nodal disease, I’m looking at stereotactic radiation. If I have bone disease, I’m looking at stereotactic. In my most unusual cases-I had a guy with solitary metastasis to the testes, and now that he’s 2 years out with an undetectable PSA, with a rising PSA previously-I’ve got, oh my gosh. It’s all anecdotal data, but we’ve seen some real spiking responses in treating minimal metastatic disease with stereotactic treatments.
So yeah, for the moment I’m stuck with that. I also introduced a concept of immunotherapy. Immunotherapy works best when there’s low-volume disease, so I like a guy with low volume to introduce the concept of immunotherapy. Once again, I’ve seen some unusual immunotherapy responses in guys with that small volume of disease. It’s all anecdotal. The problem is, I don’t have data. But I don’t know what to do with it. Without data, I’m moving ahead saying, “I’ve got something to treat.” And I’ve got enough anecdotal cases to say, “I want to continue to do that.”
Raoul Concepcion, MD, FACS: I think it’s important for the viewers to remember that right now, fluciclovine, or Axumin, is currently approved. It’s approved in the United States, and it has to be a patient who has been diagnosed with prostate cancer and has been treated. It requires no other documentation. They don’t have to be CRPC. In a lot of markets, active surveillance is considered a treatment. Currently right now, as we sit here, that is the only FDA-approved biomolecular scan. As we talk about PSMA [prostate-specific membrane antigen], we think it’s going to be on the horizon. There are all kinds of issues obviously with PSA limitations and those types of things. But I think because most of us have discussed in this segment that this is an area, there’s a lot of attention and now there are obviously new therapies that are made available to our patients. Gordon, to your point, it is the early identification that’s important.
Panelists:
- Raoul Concepcion, MD, FACS, Vanderbilt University School of Medicine, Nashville, Tennessee
- Jahan Aghalar, MD, Board-certified Hematologist and Oncologist, New York, New York
- Gordon Brown, MD, Rowan University School of Osteopathic Medicine, Glassboro, New Jersey
- Jorge Garcia, MD, Cleveland Clinic, Cleveland, Ohio; Jonathan Henderson, MD, Regional Urologist, Shreveport, Louisiana
- Paul Sieber, MD, Penn Medicine Lancaster General Hospital, WellSpan Ephrata Community Hospital, Lancaster, Pennsylvania
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.