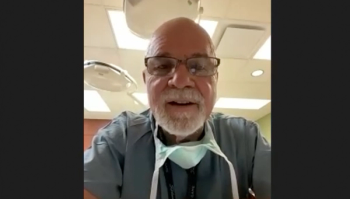
Dr. Chai discusses how physicians can resolve imposter syndrome
In this interview, Toby C. Chai, MD, discusses the main takeaways from his presentation on imposter syndrome, personal experiences with imposter syndrome, and ways that physicians can avoid and or/resolve this negative feeling.
Given the high-stress environment and competition associated with medicine, it is no surprise that imposter syndrome is experienced by many trainees and physicians.
Toby C. Chai, MD, stressed this idea in a presentation he recently gave at the Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction 2022 Winter Meeting. In this interview, he discusses the main ideas of his presentation, personal experiences with imposter syndrome, and ways that physicians can avoid and or/resolve this negative feeling. Chai is a Professor and Chair in the Department of Urology at the Boston University School of Medicine, and Chief of Urology at the Boston Medical Center in Massachusetts.
Please summarize the key points of your presentation.
Imposter syndrome was first described in 1978 from a study of women who had achieved high positions, and how their feelings of self-doubt and lack of confidence came from thinking that they got there purely by luck, or other circumstances besides their own accomplishments. I also discussed factors that contribute to imposter syndrome, how imposter syndrome negatively impacts well-being of the individual (which can result in anxiety, depression, frustration, stress and loss of work-life balance which contribute to burnout), ways to mitigate imposter syndrome, and gave my own experience with imposter syndrome.
Can you discuss a time when you have personally experienced imposter syndrome?
Imposter syndrome can occur at any time in one's career, not just during training. . I recently started my job at Boston University / Boston Medical Center in late 2019 (right before COVID pandemic) and I wondered, "Why was I selected for this job?" With my accomplishments and expertise in non-admininstrative domains, and without a MBA degree, I had some self-doubts.I wondered whether I would be able to translate the skills I’ve learned in other areas into effective administrative leadership.In short, sometimes I felt as an imposter in the position that I was in.
What are some tips and tricks that you would advise for urologists to avoid or prevent experiencing imposter syndrome?
Having good mentorship is one way to prevent and/or minimize imposter syndrome. When I started my job, I was paired with a mentor who was Chair of another department. The mentor is someone who can be a “sounding board” providing guidance and advice.Another way to reduce imposter syndrome is to work with a life coach (“executive coach”). Although this method might be only applicable for those in certain points of their careers, having an executive coach is becoming the norm for onboarding of individuals who start leadership jobs. Having the support of friends and family members can also mitigate some of the negative effects of imposter syndrome. Understanding certain characteristics that are common in surgeons (characteristics found to define surgeons from qualitative studies) can help get a better handle on imposter syndrome.For example, surgeons tend to have attitudes of perfectionism and self-critique; these attitudes can exacerbate imposter syndrome.However, other common attitudes such as self-management behavior, personal resilience, and ability to accept constructive criticism reduce the tendency for developing imposter syndrome.
What are some ways that the system at large can prevent and resolve imposter syndrome?
From a system standpoint, changing the culture of how we educate and train urologists can reduce imposter syndrome.A system level change that has helped is emphasizing the team approach in patient care, research, and education.Teamwork is emphasized early on in the educational process, so we are all familiar with the team concept. Successes (and failures too) are reflections of team efforts and not just one person, thus potentially reducing imposter syndrome. Another system effort to help reduce imposter syndrome is to ensure that good role models are provided to the trainees early on starting in medical schools. Personality traits in physician role models that were valued highly by trainees included attitudes displayed toward residents and students, compassion for patients and their familes, interaction with other healthcare workers, leadership qualities, sense of humor and social conscience. Having institutional efforts in training, recruiting and retaining these types of role models would be a way to reduce or prevent imposter syndrome. Having programs that helps maintain and promote work-life balance will also be helpful in reducing the effects of imposter syndrome. -
Is there anything else that you felt our audience should know about this topic?
There are “internal” and “external” factors that play a role in imposter syndrome.Internal factors include our faith or religion, gender, and race.External factors include our culture, ethnicity, upbringing, peer pressure and societal norms/expectations.Racism, sexism and discrimination increases the risks of developing imposter syndrome for those exposed to these societal ills. We need to be aware of how imposter syndrome can affect urologists anytime during their careers and institute mitigation efforts that will reduce burnout from imposter syndrome.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.