When it comes to urology teaching or learning opportunities, just say yes
"Despite the uncertain times, I am grateful to be a student in the field of medicine, where compassion is one of the traits that defines its practitioners," says PA student Steffanie Robertus.
Although many of the coronavirus disease 2019 (COVID-19) pandemic’s effects on daily life have made themselves known, there is still a great deal of uncertainty regarding the future. For Steffanie Robertus and Amy Pearlman, MD, dealing with this uncertainty has revolved around 1 simple word: “yes.” Robertus is a physician assistant student, and Pearlman is director of the Men’s Health Program and clinical assistant professor of urology at the University of Iowa, Iowa City.
Robertus: 2020—what a wild ride. I’ve eagerly anticipated this year for nearly a decade. This year, I was supposed to graduate from my physician assistant (PA) program with hopes of starting my first PA job somewhere in the Rocky Mountains. This was also supposed to be the year I bought a house, maybe even the year my favorite NBA team finally won the championship (Go Sixers!). Instead, I find myself unsure of when I will graduate (early 2021 is the current projection), unsure of where I will live in a few months, and unsure if I will be able to find a job in urology, or even a job at all. At least my uncertainties about the Sixers playoff performance have been put to rest (RIP).
I was several months into my clinical year when the pandemic swept the country back in March. Since then, in-person clinical rotations for my PA student colleagues and me have resumed, but the rotations and opportunities have changed. Some opportunities no longer exist, like observing and assisting with intubations, at least for the time being. While I’m grateful for the measures being taken to protect both patients and students, I feel anxious about my future post-graduation and I anticipate I am not the only one who feels this way.
As PA students, unlike medical students, most of us do not complete formal residency or fellowship training. I worry that this reduction in clinical hours may result in my being underprepared to enter the workforce. I wonder how difficult it will be to find a job as a new graduate with less experience than a typical new graduate, when the job market is already oversaturated with experienced advanced practice providers (APPs) who have been furloughed.
Despite the uncertain times, I am grateful to be a student in the field of medicine, where compassion is one of the traits that defines its practitioners. Despite their own stresses of working during a pandemic, the preceptors that I’ve been able to rotate with have all been generous with their time in teaching me and helping me find new ways to learn. Though the pandemic has put a stop to many of our traditional experiential learning opportunities, I’ve chosen to say “yes” to the “out-of-the-mask” opportunities, namely with research and curriculum development. I’ve been able to take the lead on a prospective multi-disciplinary research project with my urology physician mentor. I’ve learned how to be a better writer and communicator by preparing a grant and institutional review board (IRB) proposal and learning how to input and administer electronic patient surveys. I am also learning how to provide accessible, streamlined, and evidence-based care that incorporates guideline statements, patients’ quality-of-life goals, and clinical expertise in my current work helping to create a men’s health curriculum.
This year, opportunities for learning look different. I am learning to cope with the uncertainty. I am learning the meaning of resilience. I am saying “yes” to all learning opportunities.
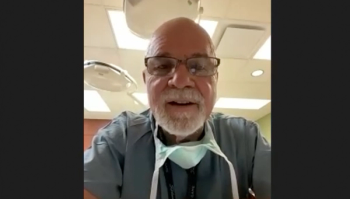
Pearlman: High-achieving students, like Steffanie, are worried about their futures and I don’t envy their current struggles. As someone who has completed her training, the days, weeks, and months, seem to blend together and the milestones of a calendar year completed don’t carry as much significance as I remember they did when I was still in training.
I worked with Steffanie for 2 weeks back in January for one of her first clinical rotations. She was brave enough to be the first PA student to sign up for my men’s health PA rotation and she was a rock star. She obtained and presented clear and concise patient stories during clinic, volunteered to come in on the weekends to round, and attended research and administrative meetings with me. She volunteered to take the lead on a prospective interdisciplinary research project I was hoping to start with the vice dean for clinical affairs. She learned how to write a grant and IRB proposal and garnered no shortage of compliments from my colleagues, who commented on her exceptional performance.
While Steffanie expresses anxiety toward her uncertain future, a completely normal response to the current circumstances, I couldn’t be more optimistic. Steffanie is a “yes” woman. She is a task doer and a communicator. These skills will serve her well and will be what makes her successful despite the current limitations with in-person clinic rotations.
I’m not sure how much interest Steffanie had in urology or men’s health prior to her rotation with me in January. I’d like to think I played some role in her desire to pursue a career in urology and, if so, it may have been simply because I provided her with opportunities to play an important role on our team.
As a community of urologists, I think we all understand the important roles that APPs play in our ability to provide accessible, streamlined care to our patients. These unprecedented times call for unprecedented educational opportunities. If we hope to encourage the next generation of APPs to pursue fields in urology, now, more than ever, we have an eager and captive audience wanting to learn what our field and specialists have to offer. I am saying “yes” to all teaching opportunities and I hope you do, too.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.