- Vol 49 No 01
- Volume 49
- Issue 01
What do you hope to see happening in urology in 2021?
"I’m just praying for it to go back to the way it was in 2019, honestly," says 1 urologist.
Urology Times® reached out to 3 urologists (selected randomly) and asked them each the following question: What do you hope to see happening in urology in 2021?
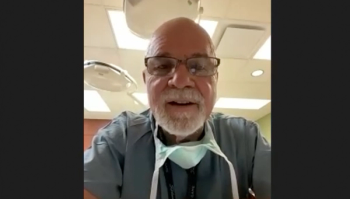
“I’m just praying for it to go back to the way it was in 2019, honestly. This year has been an exhausting, trying, difficult-to-navigate year. It would be lovely to just be the way it was a year ago. I’m not looking for anything exciting; I’m only looking to be able to practice medicine where I’m seeing patients in my office and having lunch with my staff again.
We are doing a ton of telemedicine here in Philadelphia. We’re not doing a ton of operating, but we’re doing a ton of telemedicine, which is not as fulfilling as seeing patients in the office.
I’m not hearing about a lot of advances going on in urology right now. That doesn’t mean it’s not happening; I’m just not aware of it.
At least [coronavirus disease 2019 (COVID-19)] doesn’t seem to be affecting the urologic system that we’re of aware of right now. I’m just hopeful the vaccines can get us back to normal.
This is probably about the first year we haven’t really been looking forward to some decent advancements in urology. There may be some coming, but this has been such a bizarre year [that] I think most everybody’s just looking to survive and get through this year as best we can. Our practices are changing. Patients aren’t coming in. We certainly don’t have our staff. It’s hard to look to the future when you can barely function in the present.”
Melanie Amster, MD / Philadelphia, Pennsylvania
“I’m certainly hoping, obviously, that we can return to practicing safely and helping patients with their urologic conditions in a timely manner.
We’ve had a lot of stress [around] delivering care because of COVID-19. There [have] been delays for men with prostate cancer [and for] people suffering with prolapse or other issues who are having trouble getting into, or are afraid of seeing, urologists. I really hope that doctors and their staffs can serve those people safely this year.
When they talk about elective procedures being postponed or unavailable because hospitals are dealing with COVID-19, we’re talking about the lady who has prolapse or the man with the catheter. Those are elective, but they’re definitely critical to quality of life. I’m hoping we can get back to taking care of patients who need us.
As far as anything new coming out of research, it’s actually been difficult, at least in California. We’ve had trouble because [of the] stay-at-home order. Campuses were closed; research staffs weren’t allowed on campus. In the spring, we shut down a lot of our labs.
I do health services research, so we can work remotely more easily, but it sometimes involves encountering patients. That’s a problem. I have COVID-19 right now. I’m recovering, but I was pretty sick.
Research was getting back to normal, but now we have another surge so we’re having another lockdown.
There’s been less travel and more online conferences and meetings. That’s been a big change. There’s been more time, but there have been resource constraints around doing research at many facilities where campuses are not open.
Some interesting proposals are coming up [for] managing bladder cancer; some proposals are being developed around molecular subtyping of bladder cancer. There are also proposals around handling small renal masses—how to manage them without overtreating or undertreating them and the role of biopsy in those plans.”
Christopher Saigal, MD / Los Angeles, California
“I’m excited for potential FDA approval of 2 intravascular therapies for high-risk, non–muscle invasive bladder cancer [that is] unresponsive to BCG. These include nadofaragene firadenovec, an investigational gene therapy by FerGene, and oportuzumab monatox, a recombinant fusion protein by Sesen Bio. These 2 therapies will join pembrolizumab [Keytruda], the first drug for patients unresponsive to BCG that was just approved this year that could allow these patients to avoid a cystectomy.
In prostate cancer, we should have the announcement of the phase 3 VISION trial results of the novel therapeutic drug Lu-PSMA-617, a prostate-specific membrane antigen–targeting agent used to deliver radionuclide therapy for the treatment of advanced prostate cancer patients with [metastatic castration-resistant prostate cancer]. This would add another new therapeutic with a distinct mechanism of action.
But I’m most excited about the FDA approval of the first and only oral [gonadotropin-releasing hormone] antagonist, relugolix (Orgovyx, Myovant Sciences), for androgen deprivation for patients with advanced prostate cancer. It offers enhanced cardiovascular safety and an enhanced mechanism of action as an antagonist. It has faster, more profound testosterone suppression and a shorter course of therapy.
Fortunately, our research program has not been deterred by the pandemic, and we’ve not experienced any setbacks in monitoring our patients or in accruing new subjects.
Our clinic, both outpatient and inpatient schedules, has been very busy. But personally, I haven’t been traveling anywhere near the degree I was, so it has allowed me to be more productive regarding my educational endeavors and
my research.”
Neal Shore, MD / Myrtle Beach, South Carolina
Articles in this issue
about 5 years ago
Tax code in 2021: Take note of these changesNewsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.