Dr. Helfand on escalation/de-escalation of treatment based on PSMA-PET
“I think this is really playing a role in the decision for where we're localizing our radiation therapies as well as the addition of ADT plus an androgen receptor pathway inhibitor, ARPI, and the duration of these therapies,” says Brian T. Helfand, MD, PhD.
Episodes in this series
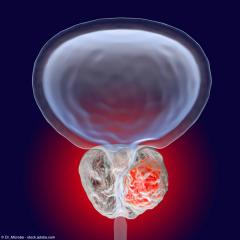
In this interview, Brian T. Helfand, MD, PhD, discusses the role of PSMA-PET imaging in tailoring treatment plans for patients with prostate cancer. Helfand is a urologic oncologist at NorthShore University Health System in Chicago, Illinois.
Video Transcript:
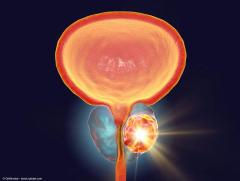
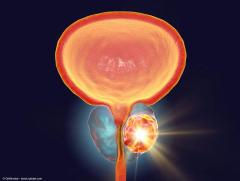
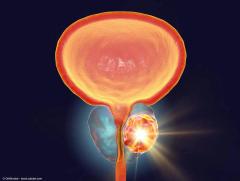
I think a lot of the trick of prostate cancer is that if we can see where the location of a tumor is, that's going to help identify where we should focus our treatment. I think that that makes sense. And certainly, [where] that comes into play is that if you only have a tumor that's localized to the prostate, that we can see even with the fanciest PSMA-PET imaging, we feel better that we may not have to treat other areas, especially when in the staging setting of a high-risk or very high-risk tumor. Certainly, when we talk about the biochemical recurrence tumor where these days, we have more focal treatments, certainly, we want to target those treatments, including SBRT, to other sites that we may see. We can intensify the treatment, so to say in those settings to say that if we have a biochemical recurrent situation where we have a rising PSA after a prostatectomy, we do a scan, and we see that there is limited uptake in the prostate bed, but there's a lymph node that may either be in the pelvis or certainly distant, we can then make our plan based on that. That plan may include an intensification and in addition to radiating the pelvis, you may actually radiate that area, if possible or feasible.
Then it also begs the question, if you see that, how much hormone therapy in the N1 or M1 or M0 type setting, and again––depending on that situation and what the images show––that you would actually offer that patient. I think it certainly adjusts that plan because again, when we know that there's disease present, especially in M1 setting, we're going to involve an intensification with more extended hormone therapies, etc. I think this is really playing a role in the decision for where we're localizing our radiation therapies as well as the addition of ADT plus an androgen receptor pathway inhibitor, ARPI, and the duration of these therapies. I think the intensification or even de-escalation when we don't see those diseases is quite appropriate and our natural reaction to those imaging results.
This transcription has been edited for clarity.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.




![EP. 9 [68Ga]Ga-PSMA-11 PET/CT shows value in initial staging of prostate cancer](https://cdn.sanity.io/images/0vv8moc6/urologytimes/6583419a0719128d5ec70eb6a2f5729faf857b50-1200x905.jpg?w=240&fit=crop&auto=format)