Dr. Spratt on the importance of a multidisciplinary approach to PSMA-PET
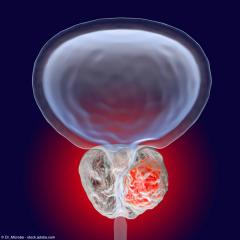
“I think that having the clinical context such as the PSA, the Gleason score, the other features that assess the aggressiveness of the disease can really help with some of these subtle findings that can be found on PET imaging,” says Daniel Spratt, MD.
Episodes in this series
In this video, Daniel Spratt, MD, discusses the critical need for a multidisciplinary approach to PSMA-PET in order to harness the full potential of the breakthrough. Spratt is the chairman and professor of radiation oncology at University Hospitals Seidman Cancer Center and Case Western Reserve University in Cleveland, Ohio.
Video Transcript:
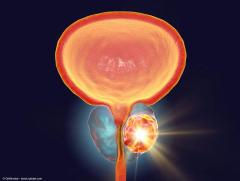
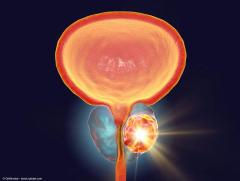
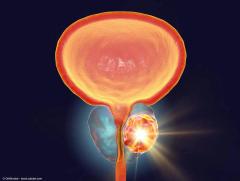
With any new treatment technology, and imaging falls right into that category, there's a big learning curve, both for the radiologist or nuclear medicine physicians to interpret and read and understand that imaging, but often, it really requires a multidisciplinary approach with the clinicians, with the surgeons or radiation oncologists or medical oncologists, because there are some unique false positives with this PSMA-PET imaging. One of the most common that we discuss a lot in our clinics is there can be subtle uptake in ribs. It's been pretty well established that most of these appear to be false positives. That low SUV uptake does not translate into these actually being metastatic sites. But if you call these as metastases, you would be giving potentially doublet or maybe, depending on other features, triplet systemic therapy, vs maybe just offering local therapy to the patient. I think that having the clinical context such as the PSA, the Gleason score, the other features that assess the aggressiveness of the disease can really help with some of these subtle findings that can be found on PET imaging.
This transcription has been edited for clarity.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.




![EP. 9 [68Ga]Ga-PSMA-11 PET/CT shows value in initial staging of prostate cancer](https://cdn.sanity.io/images/0vv8moc6/urologytimes/6583419a0719128d5ec70eb6a2f5729faf857b50-1200x905.jpg?w=240&fit=crop&auto=format)