Dr. Koontz on how PSMA-PET improves targeted treatment strategies
Key Takeaways
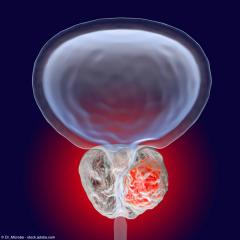
- PSMA-PET imaging enhances prostate cancer treatment by accurately identifying recurrence sites, even with PSA levels below 1 ng/mL.
- The ability to localize cancer recurrence allows for more targeted therapies, such as SBRT, improving treatment precision.
“Nowadays with PET, it's not perfect, but even with a PSA less than 1 ng/mL, we can detect the site of recurrence about 2/3 of the time,” says Bridget Koontz, MD.
Episodes in this series
In this video, Bridget F. Koontz, MD, FASTRO, highlights the role that PSMA-PET imaging has played in enabling more targeted treatment for prostate cancer. Koontz is radiation oncologist and the medical director of radiation oncology programs at AdventHealth Cancer Institute in Orlando, Florida.
Video Transcript:
The main thing is that prior to PET, we would know that there was cancer because the PSA would rise after treatment, but we didn't know where it was. What that meant is there were times where we would say,"Well, based on the clinical data that I have––based on the prostatectomy report, or your Gleason score, or the timing that it took for the PSA to recur––I think that it is most likely in this spot. It's in your prostate bed. It's in your pelvic lymph nodes." We would say, "We don't know for sure, but do you want us to give a go and try?" And actually, that's what I did for many years; that was the data we had at the time.
Nowadays with PET, it's not perfect, but even with a PSA less than 1 ng/mL, we can detect the site of recurrence about 2/3 of the time. So, that means that in 2/3 of those men, rather than treating broadly with best guess, we're able to specifically target. SBRT is a type of radiation that is very tightly focused. I'll be honest, I don't always use SBRT. Sometimes, if it's in a pelvic node, for example, I want to treat the other nodes, because if it's in that node, how did it get there? It probably traveled up the lymph node chain, and there might be other lymph nodes involved. So, I tend to treat a little bit broader. We're still getting more thoughtful about what we know about cancer [and] what we know about how prostate cancer progresses, but it has allowed us to be more targeted and more patient-specific with the treatment. That, I think, has created a whole new stage for patients. You used to have limited stage or metastatic disease, and now there's this limited volume of recurrent oligometastatic. That's where the oligometastatic came from, is the fact that we can now find the cancer before it has spread broadly.
This transcription has been edited for clarity.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.




![EP. 9 [68Ga]Ga-PSMA-11 PET/CT shows value in initial staging of prostate cancer](https://cdn.sanity.io/images/0vv8moc6/urologytimes/6583419a0719128d5ec70eb6a2f5729faf857b50-1200x905.jpg?w=240&fit=crop&auto=format)