Dr. Helfand on potential future directions with PET imaging
"Understanding that biology of that tumor and/or combining or using multiple radiotracers, either simultaneously or in sequence, may really be exciting to identify where those tumors are located," says Brian T. Helfand, MD, PhD.
Episodes in this series
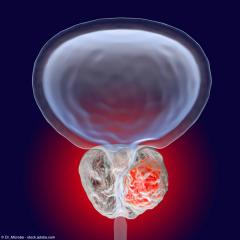
In this interview, Brian T. Helfand, MD, PhD, highlights potential advances in PSMA-PET imaging that he findings exciting. Helfand is a urologic oncologist at NorthShore University HealthSystem in Chicago, Illinois.
Video Interview:
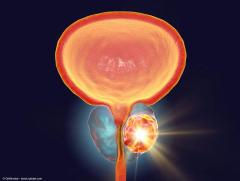
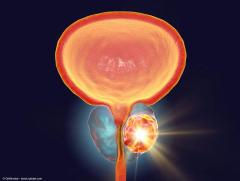
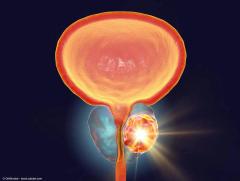
I think there's many different areas that are really exciting in the PET imaging field. Certainly, I think that the ability to become more and more sensitive is imperative. Right now, we still don't really appreciate the limits or extent of how small of a tumor we can identify. I think I previously said that right now, I think we can get to about 4 millimeters. But again, we really want to compete with pathology in that terms, meaning that if we can get the agents to be as sensitive as the microscope, then we're really hitting it out of the park. I think a lot of the newer agents that may have multiple areas that will light up, if you will, over time, that we have the ability to maybe increase our sensitivity. The other exciting area is understanding the biology. We certainly know that not all prostate tumors, and certainly in the recurrent or hormone refractory setting, are going to be PSMA-positive, or avid. As such, we may have to employ other types of radiotracers that may be more appropriate in those settings. Understanding that biology of that tumor and/or combining or using multiple radiotracers, either simultaneously or in sequence, may really be exciting to identify where those tumors are located.
I think another really exciting part of where the field is going is to say, "What other tracers should we be using? Should we be using neuroendocrine avid tracers, etc, in that same type of setting, especially when patients have been exposed to hormone therapy, etc. I'm just really excited about a lot of what is coming forth. Then I think, as previously brought up, is to say, once we understand a lot of that is what settings are most appropriate? Should we be using certain radiotracers to identify patients at the beginning of their journey when we are either screening patients or using those as decisions for active surveillance, and certainly in the staging and recurrent settings. I think the use of these agents along that patient journey is also coming into question and the appropriateness. A lot of this will also be balanced by the cost, because many of these are really expensive. We have to always keep in mind what other tools we should be using that may be either equally or more appropriately cost-effective.
This transcription has been edited for clarity.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.




![EP. 9 [68Ga]Ga-PSMA-11 PET/CT shows value in initial staging of prostate cancer](https://cdn.sanity.io/images/0vv8moc6/urologytimes/6583419a0719128d5ec70eb6a2f5729faf857b50-1200x905.jpg?w=240&fit=crop&auto=format)