Jeremie Calais, MD, on rationale for reporting template for PSMA-PET scans
Key Takeaways
- PSMA-PET/CT scans have become widely available, enhancing patient care but reducing interpretation quality outside expert centers.
- False positives, especially in bone scans, can lead to unnecessary treatments, highlighting the need for accurate interpretation.
"But as you get out of expert centers and academic sites that did it for years under research protocols, the level of the quality of the reads decreases," says Jeremie Calais, MD, PhD.
Episodes in this series
In this video, Jeremie Calais, MD, PhD, describes the rationale for the report, “Standardized template for clinical reporting of PSMA PET/CT scans.” Calais is a nuclear medicine physician at the University of California, Los Angeles.
Video Transcript:
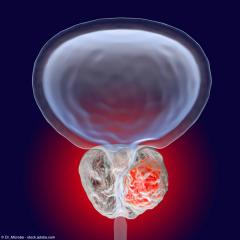
Since the FDA approval of PSMA-PET/CT back in 2020 then subsequently followed by [18F]DCFPyL PET/CT and other PSMA-PET agents that became commercially available in 2021, even 2022—now we have 5 or 6 of them available. PSMA-PET/CT got widely available and spread out in the community, which is great for patient care and urologists. But as you get out of expert centers and academic sites that did it for years under research protocols, the level of the quality of the reads decreases, of course, because not everybody can be experts in prostate cancer in the radiologists or nuclear medicine physicians. Not everybody knows what exactly to look for when you need to talk to radiologists. Maybe some imaging readers are experts in other cancers, in non-oncological disease. So, you decrease, of course, the level of expertise as you go out and spread out in the community.
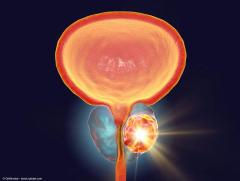
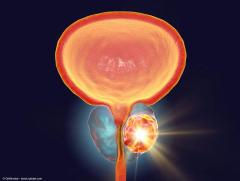
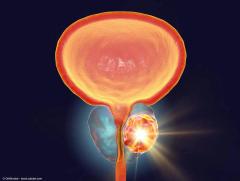
And of course, by doing that, you get more false reads, which can be false negatives, but most importantly, false positives. The false negatives are not so important at the end, just that often you cannot go really beyond the limitation of the PET technique and the detector, the spatial resolution. I think it's okay to miss a lesion—if it's small, if it's faint, it's probably either not super clinically relevant, yet, at least. What is more problematic is to have false positive findings that the urologist, the oncologist act on and treats, whereas it was not a prostate cancer-related lesion. The false positive, the main example are the bone, false positive findings that you can have all along the skeleton. But the main example are the ribs, because the ribs can be the site of unknown trauma. Some frail patients, just by coughing, they can have a little trauma on the ribs. Each trauma that will enhance a little bit of inflammation, create a bit of revascularization and healing processes can light up on a PSMA-PET scan and mimic a prostate cancer metastasis at early disease stage, when you don't see anything on the CT yet. These things are important to know. They can be also early-stage prostate cancer metastasis that when you treat it focally with radiation therapy, actually hurting the patient. You have this line; you have to make a call—is it a lesion? Is not a lesion? Should I follow it? Should I treat it? This is really something important.
Then, this is the case also for the intraprostatic reads. The overall PSMA-PET uptake in the prostate is sometimes not easy to read. You don't have the spatial resolution, the tissue resolution you get with MRI, very refined features. Here it's just blurry signal in the whole prostate. Sometimes the whole prostate is lighting up, so it's not always easy. So, you also have some techniques to use on how to read and extract information in the prostate gland itself, from the PSMA-PET information. You can still get relevant information: seminal vesicle invasion, extracapsular extension—so T3 disease—bilateral secondary lesions. You can get all that. These are, I would say, probably the main 2 pitfalls, caveat that I see in the community, when I have to do some overreads.
Then you want to make sure that everybody reports the same thing. Do not forget to look at some specific areas, even the lungs, the penile area, the brain in advanced metastatic prostate cancer patients; these can be the sites of metastasis. In fact, we rediscovered that on PSMA-PET scans. How to report the SUV, the value, talking the same language—TNM score classification is great, but some [are] not using specifically the same language, so we have criteria for that.
This transcript was AI generated and edited by human editors for clarity.
Newsletter
Stay current with the latest urology news and practice-changing insights — sign up now for the essential updates every urologist needs.




![EP. 9 [68Ga]Ga-PSMA-11 PET/CT shows value in initial staging of prostate cancer](https://cdn.sanity.io/images/0vv8moc6/urologytimes/6583419a0719128d5ec70eb6a2f5729faf857b50-1200x905.jpg?w=240&fit=crop&auto=format)